Dr. Gerald H. Smith
Dental Orthogonal Radiographic Analysis is a diagnostic record that represents an essential part of the new paradigm of dental orthopedics. Whether a practitioner utilizes the ALF System (Advanced Lightwire Functionals) or any other system that employs functional orthopedics/orthodontics, it is absolutely essential to use additional radiographic evaluation and clinical palpation of pre and post treatment changes to the cranium. Use of any functional dental appliances and/or fixed orthodontic bracket systems that alter the maxillary teeth and arch form will cause functional structural changes to the cranium, dural membrane and craniosacral systems. Since these changes occur 100% of the time, a treatment record is needed to document existing conditions of the skull and provide treatment objectives for correction. DORATM represents a new standard of care that should be exercised by all dentists in their pre-treatment orthopedic/orthodontic work-up.
The basis of the orthogonal radiographic technique is derived from the fact that structural balance of the body is maintained and self-corrects when the body exhibits the presence of right angles (Latin: Orthogonus) within its key complexes (cranium, cervical, dentition, sacrum and pelvis). The major horizontal planes: eye, ear, atlas, shoulder, and pelvic planes form right angles with a vertical mid-line reference line drawn through the full length of the body. The major horizontal planes of the skull must also demonstrate parallelism to the other planes as well as an orthogonal relationship to the vertical reference line.
The human skull is comprised of twenty-eight bones which are joined together by means of sutures. These expansion-contraction joints enable the skull plates to adjust to internal and external changes in muscles, ligaments and dural membrane tensions. The pure structural function of the osseous components of the skull are no different than those of a building, bridge or road. A mechanism for expansion-contraction must be present in all structures to prevent excess strain and damage. The positional changes of the sphenoid, temporals, malars, atlas and odontoid process can now be measured radiographically and provide the practitioner a guide in his or her orthopedic/orthodontic therapy.
Of the twenty-eight cranial bones, two have the greatest neurologic impact: sphenoid and temporal bones. The cranial nerves that pass in direct contact with these two bones represent 92% of the cranial nerves. Balance of the sphenoid bone depends primarily on the function of both the internal and external pterygoid muscles and dentition. These two muscles act as a stabilizing sling while the dentition provides the self-correcting mechanism to balance the sphenoid (fig.1) and entire cranium. The temporalis and sternocleidomastoid muscles provide the primary counterbalancing mechanism for the temporal bones. These major muscle groups are directly influenced by the vertical, transverse plane of the maxillae, alignment of the dentition, dural tube and pelvis. When the dental occlusion falls within its physiologic adaptive range of functionality (in a 3-dimensional plane), it provides the self correcting mechanism for balancing the entire structural system. When a malocclusion exists, the distortion serves to perpetuate cranial lesions (sphenoid torsion, internal or external temporal rotations, and sphenobasilar sidebends represent some of the many lesions that can exist), upper cervical instability and compensatory changes in the spine, sacrum and pelvis. With balance comes a quiet steady physiologic flow of neurologic impulses; however, with dental distortions comes a dyspenetic barrage of faulty neurologic input into the central nervous system. The immediate result is abnormal motor and sensory dysfunction, circulatory diminution, over stimulation of the adrenals and functional disturbances of muscle interlinks (temporalis-quadratus lumborum; masseter-gluteus minimus; external pterygoids-adductors [pectineus, brevis, magnus and longus]; internal pterygoid-psoas; buccinator-obturator internus). These dental muscle interlinks cause a direct affect on the stability of the pelvis and vice versa.
Orthogonal Radiographic Analysis:
To standardize the radiographic technique one must employ a head positioner that allows the technician to reproduce the patient’s head in the post-treatment record. The author has collaborated with Margraf Dental Mfg.1 to custom design a special nose positioner that permits recording of a reproducable head position. Practitioners who already have a cephalometric set-up can usually purchase a modification kit from the original manufacturer or Margraf Dental to permit A-P radiographic views. The A-P view is enhanced prior to exposure by having the patient open their mouth and align the maxillae parallel to the floor.
Anatomic landmarks (fig.2) and reference lines (fig.3):
- VRL (Vertical Reference Line): Vertical line drawn through the center of nasion and the anterior nasal spine.
- LWS (Lesser Wing of Sphenoid): Horizontal line connecting the height of convexity of the right and left portions of the lesser wings of the sphenoids.
- AT (Apex of Temporal Bones): Horizontal line connecting the tips of the right and left apices of the petrous ridges.
- ML (Malar Line): Horizontal line connecting the inferior borders of the right and left malar (zygomatic) bones. This line also provides a clue as to the cant of the maxillae.
Interpretation of distorted landmarks:
Lines above the corrected horizontal on the left side of the vertical reference line are noted in positive degrees; those falling below are noted as negative. A plus or minus of 2 degress is within the physiologic adaptive range. Three to five degrees represents minimal distortions while 6 to 7 degrees notes moderate and 8 degrees plus or minus readings are indicative of severe lesions (fig. 3). These radiograph findings must be correlated with palapation of the clinical cranial indicators for a more accurate 3-dimensional assessment.
Attention must also be paid to the nasal septum, turbinate spaces and shape of the hard palate as exhibited on the study casts. Distortions of the hard palate may provide a clue to possible tonsil enlargement with accompanying compensatory deviations of the tongue. This information will enhance one’s documentation, accuracy in treatment planning (possible necessity for pre-treatment tonsil removal) and if present make one aware of the need to correct cranial distortions.
For those patients who present a history of chronic pain, it behooves the practitioner to have an orthogonal chiropractor2 perform an orthogonal radiographic analysis of the atlas and occiput. If the atlas is distorted by lateral displacement and/or rotation, your chances of successfully resolving the patient’s structural TMJ problem are minimal. And one’s chances of exacerbating their symptoms are even greater since making changes to the patient’s vertical and sagittal jaw positions will tension an already tensioned dural membrane.
The dura passes through the foramen magnum and attaches tenaciously to the superior posterior ring of the atlas, bodies of the axis and sometimes C-3. The dura continues down the spine with its final attachment at the second sacral tubercle. In reality, the dental complex is intricately involved with the sacrum, spine, cervical vertebrae, central and peripheral nervous systems, and cranial bones via the dural tube 3.
Learning to palpate the cranial indicators is absolutely essential in guiding one’s orthopedic appliance adjustments. Adjusting orthopedic appliances without knowing its impact on the patient’s skull bones can have far reaching neurologic consequences. Also one must learn the significance of these cranial lesions to further assist in case analysis and appliance design. The ALF functional appliances are the only light wire appliances that can correct specific cranial lesions. Existing acrylic orthopedic appliances with expansion screws are obsolete in light of this advanced orthopedic breakthrough.
Summary
The documentation of cranial lesions will dictate the changes that must be accomplished in order to achieve a successful orthopedic/orthodontic result. The DORA system offers a means of documenting this vital component of orthopedic treatment. Coupled with the ALF Orthopedic System, this radiographic analysis and documentation improves the quality of patient care and serves to continue the advancement of the specialty of functional orthodontics. In reality anyone who performs orthopedic procedures is directly affecting the neurophysiology of the entire patient. This is an awesome responsibility and should not be taken lightly and must be treated with a full understanding of the craniosacral system.
- 611 Harper Ave.; Jenkintown, Pennsylvania 19046 ~ (215) 884-0369
- To locate an orthogonal chiropractor nearest you contact Dr. Roy W. Sweat’s office; 3274 Buckeye Rd. N.E.; Atlanta GA 30341 ~ (770) 457-4430.
- DeJarnette, Major, DC. “Sacro Occipital Technique 1981”, Nebraska City, Nebraska, published by Major Bertrand DeJarnette, 1982.

Figure 1.
The internal and external pterygoid muscles play a major role in balancing the spenoid bone. An existing malocclusion distorts the tensions applied on the pterygoid plates causing cranial lesions (greater wing of the sphenoid is either high right or left or rotated in a horizontal axis.
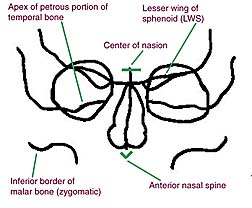
Figure 2.
The A-P radiographic view permits analysis of parallel planes which indicate structural balance. These indicators are essential in diagnosis, treatment planning and ALF design. Cranial lesions dictate immediate correction followed by corrections of maxillary cants (transverse and /or sagittal) and finally alignment of the teeth to stabilize the entire craniosacral mechanism.
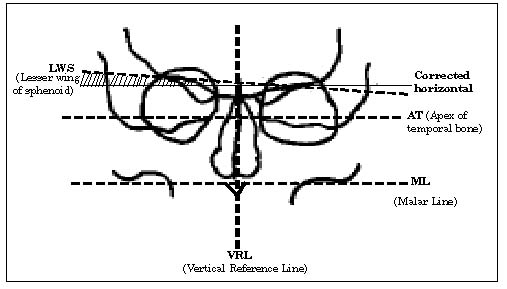
Figure 3
Instructions for placement of orthogonal reference lines:
The clinician first draws the vertical reference line: line connecting the center of the nasion and anterior nasal spine. Next draw connecting horizontal reference lines between the following points: most convex portion of the lesser wing of the sphenoids; the apecies of the petrous portion of the temporal bones; and the inferior borders of the malars. Lastly draw corrected horizontal lines (90 degrees to the vertical reference line) for each of the three lines and measure the degrees off of the corrected horizontal reference. All measurements are made on the left side of the reference line. If the connecting line is above the corrected horizontal the discrepancy is noted in positive degrees; if below the corrected horizontal the discrepancy is noted in negative degrees. Example: the LWS in the above illustration is + 5 degrees. The +5 degree discrepancy documents a high sphenoid on the patient’s left side. Since the radiographic analysis is only a two dimensional record it must be correlated with the palpatory findings to assess the acutal 3-dimensional lesion pattern. These documented findings provide a guide in understanding the patient’s total cranial lesion. It also helps guide the clinician in adjusting the ALF appliances to correct the foundation of the human skull- maxillae.
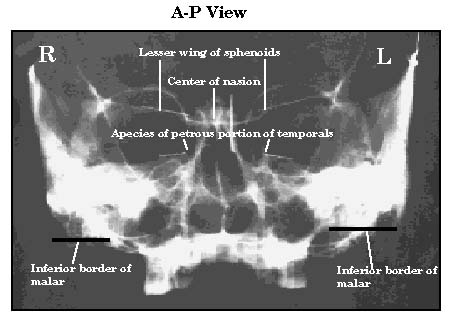
A-P Radiographic view of a dried skull with landmarks noted.
This specimen exhibits a high left sphenoid, high right apex of petrous portion of temporal bone (external rotation), high left malar with the maxillae canting up on the left side. The septum is deviated with an enlarged right turbinate.
Treatment with the ALF system focuses on first correcting the cranial lesions, second correcting the cant of the maxillae and third alignment of the teeth to stabilize and support the cranium. If these cranial distortions are allowed to remain and just the teeth jiggled into position, the case will replase and the muscles will remain in a state of imbalance. How can the mandibular condyles function properly when the maxillae is distorted, the mandible is compensating because of the maillary cant, the musculature and ligaments are functioning at different lengths and the glenoid fossae are in abnormal planes? What kind of service has the practioner provided the patient? Surgery can never fix the underlying cranial distorsions it will only serve to make a bad situation even worse.

