Sheryl Lynn Oleski, B.S., Gerald H. Smith, D.D.S., William T. Crow, D.O.
From: Cranio: The Jornal of Craniomandibular Practice, January 2002, Volume 20, Number 1, pp 34.

Abstract: The purpose of this retrospective chart review was to determine if external manipulation of the cranium alters selected parameters of the cranial vault and base that can be visualized and measured on x-ray. Twelve adult patient charts were randomly selected to include patients who had received cranial vault manipulation treatment with a pre- and post-treatment x-ray taken with the head in a fixed positioning device. The degree of change in angle between various specified cranial landmarks as visualized on x-ray was measured. The mean angle of change measured at the atlas was 2.58 degrees, at the mastoid was 1.66 degrees, at the malar line was 1.25 degrees, at the sphenoid was 2.42 degrees, and at the temporal line was 1.75 degrees. 91.6% of patients exhibited differences in measurement at 3 or more sites. This study concludes that cranial bone mobility can be documented and measured on x-ray.
Osteopathic physicians have long believed that the bones of the cranium are mobile. Unfortunately, there have only been a few scientific papers to support this hypothesis, and the palpatory findings of cranial movement are considered to be subjective. This study was designed to determine whether this cranial bone mobility could be visualized and measured on A-P radiographs.
Kragt, et al, (1) showed that movement was possible at the sutures in a macerated human skull, and Retzlaff, et al,(2) documented that the cranial sutures do not fuse with age. Taking this information a step further, Zanakis, et al,(3) attached infrared markers to the skin over selected skull bones, and used a 3-D kinematic system to analyze individual bone motion. Motion of the cranial bones was labeled complex, involving more than one axis of movement and not a simple hinge-operation.
In 1970, Greenman (4) published an article in which he described a method to diagnose cranial dysfunctions with an e-ray of the cranium. With a set of specified landmarks, and a vertical axis, torsions, and sprains could be viewed as deviations from the horizontal plane. It was also noted that a good clinical correlation existed between the x-ray findings and the palpators’ diagnoses. The landmarks and practices Greenman used are those from which the protocol for this study was derived.
Demonstrating scientific evidence of cranial suture movement in living humans has many implications for future treatments and diagnoses. These cranial manipulations are administered by the practitioner applying gentle forces with the hands to the dysfunctional regions of the patient’s cranium. In fact, many cranial manipulation diagnostic findings have already been revealed.
For example, Greenman and McPartland (5) determined that the average cranial rhythmic impulse was low when at least one strain pattern was present, and one or more bony restrictions were evident in patients with a traumatic brain injury. They believed cranial manipulation to correct these dysfunctions would aid in the treatment of traumatic brain injury. Also, Gregory (6) noted that temporomandibular disorder (TMD) was improved following chiropractic sacro-occipital technique treatment and that concurrent chiropractic and dental treatments may improve the success rate of TMD resolution.
Temporomandibular disorder was also studied by Chinappi and Getzoff, (7) who concluded that the disorder was worsened by an instability of the sacroiliac joint, specific thoracic and cervical vertebral subluxations, and cranial suture restrictions. It was improved by adjustments of the spine, neck, and cranial sutures several times a week.
Since the implications for treatment with cranial manipulation appear beneficial, the methods of diagnosis and a means to follow progress require more study. Therefore, we propose to show that cranial bone mobility can be documented and measured on x-ray.
Materials and Methods
Patient charts from a private dental office were randomly selected. These charts were subsequently reviewed to determine whether the patient met the inclusion criteria. In order to be included in this study, the patient chart needed to include two separate A-P radiographs of the patient’s head wile in a fixed head positioning device. The patients were required to be over the age of eighteen to eliminate the possibility of craniofacial changes related to normal growth and development. Also, documentation was needed to determine if cranial manipulative treatment was provided to the patient at a time between the first and second A-P radiographs. The authors retrospectively studied the x-rays of these twelve randomly selected adult patients who received cranial manipulation as part of their standard dental care regimen. Exclusion criteria included patients under the age of eighteen, patients with a history of surgery on the cranium, ears, or jaw, or cases in which there were no before-treatment and after-treatment x-rays available. In this study, none of the charts selected were excluded. The study was reviewed and approved by the institutional review board at the Philadelphia College of Osteopathic Medicine, Philadelphia, Pennsylvania.
Experimental Protocol
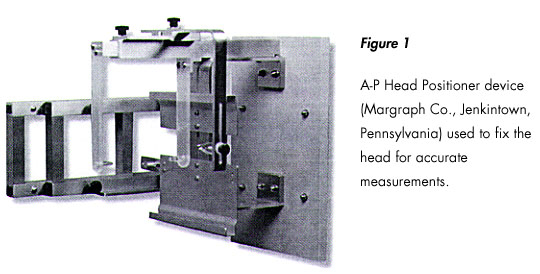
In order to determine changes in the bony parameters of the skull, it is necessary to fix the head in a positioning device for accurate comparisons of radiographs over time. The cranial fixation device that had been used in taking the x-rays was the Dental Orthogonal Radiographic Analysis method (Margraf Co., Jenkintown, PA) which requires the following equipment: cephalometric holder modified for A-P view (Figure 1); cassette, intensifying screen and grid; eyeglass frame positioner; polyflex registration material molded t the shape of the bridge of the patient’s nose; and 90 Kv x-ray unit.
After the eyeglass frame with custom molded nosepiece had been placed on the patient, the cassette and grid sheet were placed on the patient, the cassette and grid sheet into the cassette holder. The patient’s head was positioned in the A-P holder and the ear positioners were secured. The patient’s head was aligned so that the maxilla was parallel to the floor when the mouth was opened to its maximum position. At this head position the trombone rods of the eye glass frame were extended until they touched the grid sheets. Their position was marked with two ink dots where the metal rods touched the paper grid sheet. After taking the exposure, the length of each rod was measured and the number was entered in the appropriate block on the grid sheet. To insure accuracy the locator glasses were left in position while the x-ray was taken. The frame does not interfere with the analysis of the radiograph.
After the first radiograph was taken, the patient was treated with cranial manipulation by the author (GS). The treatments were customized to the patients and were not standardized throughout. Since the scope of this investigation was to determine whether cranial bone movement could be documented and measured on x-ray, the specific cranial manipulations administered to the patients are not important. After cranial manipulation was administered, the patient received a second A-P radiograph.
To take the second A-P radiograph for treatment comparison, the eyeglass frame was placed back on the patient. The film cassette with the previously marked grid sheet was placed in position. The patient’s head was placed in position with the trombone extensions pulled out to the previous measurements making sure they touched the previously marked dots on the grid sheet. The patient was instructed to open his mouth to the maximum position and the exposure was made.
For analysis of the radiograph, a vertical reference line was drawn from the center of the nasion to the tip of the anterior nasal spine using a clear plastic ruler. The vertical reference line bisected the odontoid process along its long axis.
The horizontal plane of the atlas was determined by drawing a line through the two lowest points on the lateral masses of the atlas vertebra. The angle it made with the vertical reference line was measured in degrees with a clear plastic protractor.
The inferior border of the mastoid plane was determined by drawing a line through the two lowest points on the mastoid bones. The angle it made with the vertical reference line was measured in degrees with the protractor.
The malar plane line was determined by drawing a line through the two lowest points on the inferior border of the malar bone. The angle it made with the vertical reference line was measured in degrees with the protractor.
The apex of the temporal bone was determined by drawing a line through the two highest points on the petrous portion of the temporal bones. The angle the line made with the vertical reference line was measured in degrees with the protractor.
The lesser wing of the sphenoid was determined by drawing a line through the two points where it contacted the outer rim of the orbit. The angle the line made with the vertical reference line was measured in degrees with the protractor.
To assess for interobserver reliability, these measurements which were made by the author (SO) were independently compared to measurements charted previously by the dental office staff and were determined to be accurate within 0.5 degrees. The measurements from both sets of A-P radiographs were then compared and analyzed for before-treatment and after-treatment differences.
Statistical Analysis
A D’Agostini test was performed to determine if the change in degree of measurement at the various anatomical landmarks was distributed normally. If the distribution was normal, a simple t-test was performed using the null hypothesis. When the data was not distributed normally, a symmetry and median test was performed, using the null hypothesis, to assess for statistic significance. Finally, a regression analysis was run to determine correlation between the percentage of patients with changes at certain numbers of measurement locations.
Results
The mean angle of change measured off the vertical reference line at the atlas was 2.58 degrees with a range from 0 degrees to 6 degrees. The t-test calculated p<0.01 with n=12, ny=11, and t=5.17. the mean angle of change measured at the Mastoid was 1.66 degrees with a range from 0 to 3 degrees. The t-test showed p<0.01 with n=12, ny=11, and t=3.25. At the malar line, the degree of change was 1.25 degrees with a range from 0 to 4 degrees. The abnormally nonsymmetrically distributed data yielded a p<0.01 via the median test. The mean angle of change measured at the sphenoid was 2.42 degrees with a range from 0 to 8 degrees. Again, these data were not normally distributed and were asymmetrical. The median test yielded p<0.01. At the temporal line, the mean was 1.75 degrees with a range from 0 to 5 degrees. The median test yielded p<0.01, (Table 1).
The percentage of patients with changes at the various specified landmarks fluctuated (Table 1). The percentage with change at the atlas, sphenoid, and temporal line was 91.6%. The percentage with change at the malar line was 81.8%, and the percentage with change at the mastoid only 66.6%.
The percentage of patients with a change at all five landmarks was 41.6%. While the percentage of patients with a change at three or more landmarks was 91.6%, 100% of the patients exhibited change in at least two landmarks. The regression analysis yielded a p=0.06.
Discussion
This is the first study to determine that cranial mobility can be visualized and measured on x-ray. It yielded the interesting finding that cranial mobility can be quantified. The amount of change measured ranged up to eight degrees which is fairly significant since Kostopoulos and Keramidas8 only noted a relative elongation of the falx of 1.44 mm during a frontal lift technique and measurement errors typically account for only a maximum of three degrees of difference.
While the tools used to measure the degrees of change in this study may appear rudimentary in this age of computers, they provided consistent measurements between those charted in the dental office records and those generated by the author. The authors recommend the use of architectural software with digitally scanned radiographs for future studies of this type so as to allow quantification of smaller degrees of change among landmarks and to minimize measurement errors.The change in landmarks is not likely due to chance since the radiographs were taken of the head in the fixation device. Also, since 58.4% of patients exhibited no change in measurement of at least one landmark, it appears unlikely that head positioning is a factor.
Furthermore, we discovered that the malar bone, or cheekbone, is likely to exhibit the least amount of movement whereas the atlas exhibits the greatest amount. This was not surprising since the atlas, as the first vertebrae, has a great capacity for movement and is biomechanically influenced by the rest of the spine.
Since the malar bone exhibited the least amount of movement, it would stand to reason that it has fewer interdigitated sutures. This conclusion was reached with the knowledge that Jaslow(9) noted a greater bending strength in segments of cranial bone having highly interdigitated sutures. More studies would need to be completed to determine if this is the exact reason the malar bone exhibited the least amount of movement in our study.
Table 1
| Measures | Atlas | Mastoid | Malar | Spehnoid | Temporal |
| Average degree of change | 2.58 | 1.66 | 1.25 | 2.42 | 1.75 |
| Percentage w/change | 91.6 | 66.6 | 81.8 | 91.6 | 91.6 |
| Range of degree of change | 0-6 | 0-6 | 0-4 | 0-8 | 0-5 |
Conclusion
This pilot study supports the observation that cranial mobility can be recorded and measured on x-ray. No control group was used in this study as it was performed retrospectively. The authors do not believe this is problematic since this study was only looking to determine whether movement could be documented and measured on x-ray and not to compare the cranial bone motion at rest to that generated by cranial manipulation. The authors believe these novel findings require further investigation and confirmation. The authors recommend a large scale double-blind prospective study using digital radiographs analyzed by architectural software for further investigations.
Understanding that the bones of the cranium have mobility and having a method of documenting this motion will provide evidence for numerous cranial manipulative treatment modalities. As evidenced in the literature, these treatments have the capacity to ease discomfort of temporomandibular joint disorder, traumatic brain injuries, headaches, and other somatic dysfunctions.
References
- Kragt G. Bosch JJ, Borsboom PCF: Measurement of bone displacement in a macerated human skull induced by orthodontic forces; a holographic study. J Biomechanics 1979; 12:905-910.
- Retzlaff EW, Upledger J. Mitchell FL, Jr.: Age related changes in human cranial sutures, Anatomical Records 1979; 663.
- Zanakis MF, Morgan M. Storch I, Bele M, Carpentieri A, Germano J: Detailed study of cranial bone motion in man. JAOA 1996; 96:552.
- Greenman PE: Roentgen findings in the craniosacral mechanism. JAOA 1970; 70:1-12.
- Greenman PE, McPartland JM: Cranial findings and iatrogenesis from cranial manipulation in patients with traumatic brain syndrome. JAOA 1996; 95:182-192.
- Gregory TM: Temporomandibular disorder associated with sacroiliac sprain. J Manipulative Physiol Ther 1993; 16:256-265.
- Chinappi AS Jr, Getzoff H: The dental-chiropractic cotreatment of structural disorders of the jaw and temporomandibular joint dysfunction. J Manipulative Physiol Ther 1995; 18:476-481.
- Kostopoulos DC, Keramidas G: Changes in elongation of falx cerebri during craniosacral therapy techniques applied on the skull of an embalmed cadaver. J. Craniomandib Pract 1112; 10;9-12.
- Jaslow CR: Mechanical properties of cranial sutures. J Biomechanics 1990; 4:313-321.
Ms. Sheryl Lynn Oleski is a senior medical student at the Philadelphia College of Osteopathic Medicine. She is currently completing an undergraduate fellowship in Osteopathic Manipulative Medicine and is actively involved in research. Ms. Oleski plans to pursue a residency in Physical Medicine and Rehabilitation upon graduation.
Dr. Gerald H. Smith is a D.D.S. and the author of “Cranial-Dental-Sacral Complex: First to Integrate Chiropractic, Osteopathic, Dental, Physical Therapy and Nutritional Concepts” and “Headaches Aren’t Forever.” He maintains a private dental practice in Langhorne, Pennsylvania, with a special interest in orthodontics, TMJ, and alternative dentistry. Dr. Smith has gleaned honors as an international lecturer on TMJ disorders.

