Dental/Rheumatoid Arthritis Connection
MT is a 64-year-old Caucasian female who works as a medical transcriptionist. In 1974, a diagnosis of rheumatoid arthritis was made. At the early age of 30, she presented clinical symptoms of swollen knees. Through the years, her condition gradually worsened until she experienced severe painful joints throughout her body. MT’s medical treatment included the use of the steroid, prednisone, a chemotherapy drug, methotrexate, and a deactivating drug, Enbrel. The yearly cost for just the Enbrel alone was $13,500, which was paid for by her insurance company.
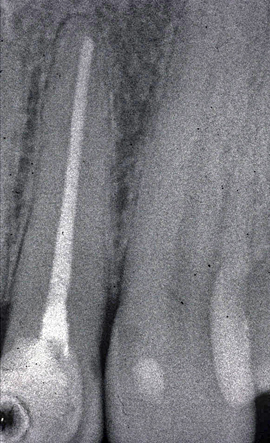
infections in dentinal tubules.
Rheumatoid arthritis affects millions of Americans. It is considered a chronic joint disease that causes the soft tissue around joints to thicken and swell and cartilage to erode. Unlike osteoarthritis, which is characterized by joint damage from wear-and-tear stress, rheumatoid arthritis (RA) is a disease in which the body’s own immune system attacks the joints, especially joints of the hands and feet. It is for this reason RA is thought to be an autoimmune disease.
Enbrel is primarily used to block the tumor necrosis factor alpha (TNF alpha), which the body produces during the inflammatory response, that is, the body’s reaction to injury. TNF alpha promotes the inflammation and its associated fever and signs (pain, tenderness, and swelling) in several inflammatory conditions including rheumatoid arthritis. From a healing perspective, inflammation is the first step in the body’s attempt to heal. Whether bacterial, viruses, fungi or chemical substances concentrate in an area the body must react to remove the offending agent(s). From a clinical perspective, it is totally illogical for the body to initiate a process that would attack itself for no good reason. In fact most “autoimmune” diseases have an underlying factor, which traditional medicine has not yet been able to recognize.
One over looked source for initiating rheumatoid arthritis are dental foci. Dental infections whether from an infected root canal tooth, gum disease or sites of previously extracted teeth all provide the potential of 300 to 400 different pathogens. Bacteria, viruses and fungi or any combination plus degenerating protein substances from tooth structures produce toxins (thiol ethers) which circulate throughout the entire body. Concentration of poisonous substances within a knee, hand, finger or other joint will cause inflammation. This was true in MT’s case. Within one to two years before the onset of her RA, she had a root canal treatment performed on an upper left lateral incisor. This seemingly innocuous dental procedure resulted in a streptococcus inflection that remained present for 34 years. An x-ray of the treated tooth showed no visible pathology. Unfortunately a high percentage of root canal treated teeth (75 percent or more) become infected, exhibit none of the usual clinical signs and symptoms of pain, swelling or redness yet spew out their toxic waste products that affect distant sites.
A noninvasive approach utilizing technology developed in the 1930’s was used to resolve the streptococcal infection within the tooth. Following two treatment sessions, MT’s rheumatoid arthritis resolved by 90% and she stopped taking the Enbrel. No additional therapy was instituted at the time of treatment. This patient has regained a pain free quality of life. The key factor was the removal of the underlying cause — infected root canal tooth — which started the release of the tumor necrosis factor.
Use of medications to block TNF (tumor necrosis factor) or any other components of the inflammatory process only treats the symptom NOT the actual cause. The belief of an “auto-immune” component of the disease process is often used because physicians do not understand the nature of the dental component in the disease process.
One over looked source for initiating rheumatoid arthritis are dental foci.

STAY INFORMED
Big tech and mainstream media try to suppress the powerful information I have to share. Subscribe here to stay informed!
